
Most people get a standard set of blood work done every year through their primary care provider, which usually includes a Fasting Blood Glucose (FBG) test. This test measures the amount of sugar floating around in your blood at the moment the sample is taken. Many providers require you to be fasted (not eating for 8-12 hours) before this test because, ideally, your fasting blood sugar should be below 99 mg/dL. However, this is just one small piece of the blood sugar picture.
To truly understand how well your body is regulating blood sugar, it is crucial to also test Hemoglobin A1c (which provides a 3-month average of blood sugar regulation) and Insulin (the hormone responsible for transporting sugar from the blood into your cells). These three tests together form the foundation of blood sugar assessment, and none should be omitted if you want to really begin to understand your blood sugar regulation and how it plays a role in your overall metabolic health.
Understanding the Three Key Tests
- Fasting Blood Glucose (FBG): Should be below 99 mg/dL, but most of my healthiest patients have readings in the low-to-mid 80s.
- Hemoglobin A1c (HbA1c): Should be under 5.7% (5.7% is the cutoff for prediabetes, and 6.5% for diabetes), though my healthiest patients typically fall between 4.8-5.2%.
- Fasting Insulin: Should be below 10 uIU/mL.
Over the 9 years I’ve been in practice, I’ve worked with many patients who have normal FBG and HbA1c but elevated insulin. This signals that their pancreas is working overtime to keep blood sugar in check—a warning sign of potential future issues. Unfortunately, most conventional practices do not test insulin unless FBG or HbA1c are high, which means problems may not be detected until they are already more serious.
The Blood Sugar Story: A Helpful Analogy
Every time you eat, your body breaks food down into glucose, the primary fuel for your cells. When the food is broken down to glucose, it’s essentially sitting around like little glucose packages in your blood stream, waiting to be delivered to your cells, and your cells use glucose to do all their daily cellular tasks. Your pancreas acts like a post office, sending out insulin postal workers to deliver glucose packages to your cells. Each cell has an insulin receptor (a doorbell) that allows glucose to enter when the insulin postal worker rings the doorbell to deliver the glucose package.
- Glucose (aka sugar) = glucose packages
- Pancreas = post office
- Insulin = postal workers
- Insulin Receptor = cellular doorbell

As your body processes the food you eat, it converts it into glucose packages that cause your blood sugar to rise. This alerts your pancreas post office to release insulin postal workers to shuttle the glucose packages into your cells, bringing your blood sugar back down. This cycle repeats throughout the day, across every day.
When Things Go Wrong: Insulin Resistance
If blood sugar is constantly high—whether from frequent eating, stress, alcohol, poor dietary choices, hormone shifts, other medications—your pancreas post office must release more insulin postal workers to manage the increased glucose packages. This is like it’s working overtime for the holidays.
Now imagine, you’re a cell and the doorbell is getting rung every hour with more and more deliveries of the same package. After a little while, you probably don’t want anymore packages because you have enough. So the cells say, “No, thank you” and they shut the door without accepting the package. But the insulin postal worker has a job to do, so they start ringing the doorbell over and over and over again. And eventually the cell gets annoyed and decides to uninstall the doorbell so it doesn’t have to hear it ring anymore. The cells are starting to reject insulin’s signal (they stop answering the doorbell), leading to insulin resistance.
Once the doorbells start getting uninstalled, this puts the insulin postal worker at a loss as to what to do, so post office pancreas sends out more insulin postal workers, thinking that while one knocks on the door, another can bang on the windows and another can try to slip a glucose package in through the chimney – this is why insulin levels start going higher and higher as insulin resistance progresses.
But how would you know this? FBG, HbA1c, and insulin may give you some initial insight to things being amiss, but they can’t tell you the whole story. This is where additional metabolic testing becomes essential.
Digging Deeper: HOMA Testing
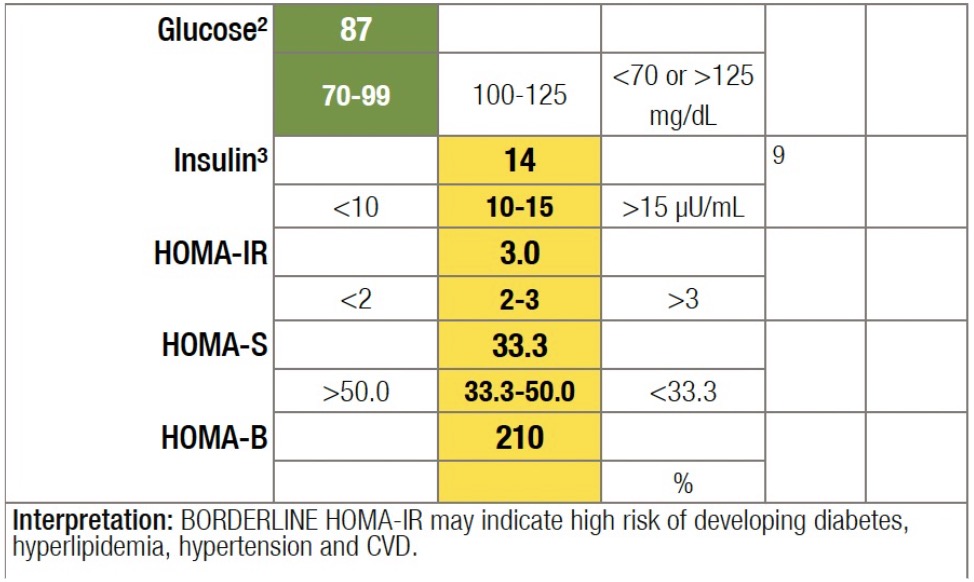
If I see any irregularities in FBG, HbA1c, or insulin, I like to run HOMA-IR, HOMA-S, and HOMA-B tests to assess metabolic function:
- HOMA-IR (Insulin Resistance Index): Measures how many cells are no longer responding to insulin (how many have “uninstalled the doorbell”). A healthy number is under 2, and a result above 3 signals significant signs of insulin resistance (even if it’s still early signs).
- HOMA-S (Insulin Sensitivity Index): Measures what percentage of cells are still responding to insulin, or still have the doorbell installed. This should be above 50%.
- HOMA-B (Beta Cell Function): Measures how hard your pancreas post office is working to get those glucose packages delivered and maintain blood sugar balance. If the pancreas is overworked, it may eventually burn out. A really high percentage (over 100%) can tell us the pancreas is working overtime, and as this number drops, especially if it’s dropping well below 100%, then we may be looking at signs of postal worker burnout and post office dysfunction.
I’m also typically recommending my patients get a Coronary Calcium Screening with an imaging center that offers Ultra Fast CT imaging. This is because, in my opinion, sugar dysregulation is more of a contributing factor to coronary artery disease than lipids. However, this is another topic for another day.
Why This Matters for Your Health
If the doorbells aren’t installed, and the insulin postal workers can’t deliver the glucose packages to the cells due
to developing insulin resistance, they have to put it somewhere so they put it into the “undeliverable storage area” AKA your fat cells. This can make weight loss difficult despite healthy eating and exercise. Meanwhile, cells that lack enough glucose because they’ve burned through their glucose packages and don’t have a doorbell to receive more, begin signaling your brain with hunger and cravings, leading to further blood sugar spikes and worsening metabolic dysfunction.
Taking Action Before It’s Too Late
I consider this testing a critical part of my baseline workup for patients. It provides a peek behind the blood-sugar-regulation curtain and can tell us how far into this process you are long before it will show up as pre-diabetes or diabetes on your standard FBG and HbA1c labs. With the right interventions—dietary changes, targeted physical activity, and personalized supplements—most patients see improvements in just three months, often avoiding the need for medication. Patients who are committed to these protocols move away from pre-diabetes, experience more optimized metabolic health on all levels, and they gain more peace of mind about their long term health goals.
If you’re interested in understanding your blood sugar story, give us a call to set up an appointment. Prevention is always better than treatment.
Know someone who could benefit from this knowledge? Share this with two people and help them take control of their health!
This post was written by Dr. Kelsey Asplin



